Superficial Cervical Plexus
Indications
INDICATIONS
Anaesthesia anterior neck and cape of shoulder, anterior neck surgery and shoulder surgery (super cial cervical plexus is often blocked with classical interscalene brachial plexus block).
Anatomy
ANATOMY
The superficial cervical plexus supplies sensation to the neck and shoulder. It is formed from the anterior rami of C2-C4 nerve roots. The branches of the plexus pierce the cervical fascia to emerge posterior to the mid-point of sternocleidomastoid muscle.
The sensory branches of the superficial cervical plexus are the lesser occipital, greater auricular, transverse cervical and supraclavicular nerves.
Landmarks
LANDMARKS
Posterior border of sternocleidomastoid muscle, mastoid process, suprasternal notch.
Positioning
POSITIONING
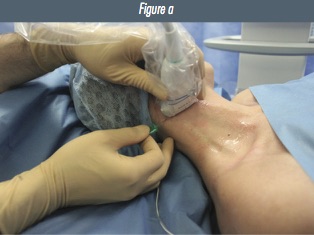
Patient supine, head turned to the contralateral side. Transducer initially applied at the level of the cricoid cartilage in the axial, oblique plane. Similar to the positioning for an interscalene block.
Figure 1: a) patient, transducer and needle positioning for in-plane superficial cervical plexus block.
Preliminary Scan
PRELIMINARY SCAN
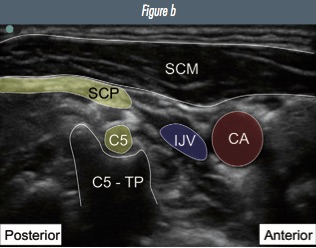
From the level of the cricoid cartilage, identify the interscalene groove and brachial plexus. Scan cranially and observe the C6 and then C5 nerve roots move deep towards their respective transverse processes (see interscalene chapter for images). At the level of the C5 transverse process, the superficial cervical plexus can be seen superficially as a line of hyperechoic beads in the fascial plane deep to the SCM muscle.
Figure 2: Ultrasound image of a) superficial cervical plexus b) annotated image (CA=carotid artery; IJV=internal jugular vein; C5-TP=C5 transverse process; C5=C5 nerve root; SCP=super cial cervical plexus; SCM=sternocleidomastoid muscle).
Ultrasound Appearance
ULTRASOUND APPEARANCE
Small hyperechoic beads superior and super cial to C5 transverse process, deep to sternocleidomastoid posterior border. May be difficult to visualise the individual nerves.
Technique
TECHNIQUE
Insert the needle posterior to the transducer using an in-plane approach (from posterior
to anterior). Injection of local anaesthetic should fill the fascial plane deep to the sternocleidomastoid muscle and be seen to spread freely towards the internal jugular vein.
|
Positioning |
Supine, head turned to contralateral side |
|
Transducer |
High frequency linear probe |
|
Depth |
1–2 cm |
|
Needle |
22-G 50 mm |
|
Plane |
Transverse |
|
Needle approach |
In-plane (posterior) |
|
Injection |
5–10 ml |
Tips
TIPS
1. It can often be quite tough to advance the needle in the fascial plane deep to the sternocleidomastoid muscle. Gentle pressure and hydrodissection may help.
2. When performing the block for carotid surgery the needle can be advanced slowly, under direct vision, towards the jugular vein and carotid artery to deposit local anaesthetic adjacent to the carotid sheath. This is often referred to as an intermediate cervical plexus block.
DEEP CERVICAL PLEXUS BLOCK
Individual cervical root blocks as performed with a classical deep cervical plexus block is not necessary and carries the risk of vertebral artery or subarachnoid injection. Ultrasound-guided superficial cervical plexus block combined with ultrasound-guided infiltration around the carotid sheath (intermediate cervical plexus block) at the level of the carotid bifurcation will provide adequate anaesthesia in around 90% of patients.
TIPS FOR CAROTID ANAESTHESIA
• Around 10% of patients will require supplementation with local anaesthetic at the angle of the jaw if the carotid bifurcation is high and a lot of surgical retraction is needed.
-
Minimal pressure must be applied with the transducer to:
i) ensure the jugular vein is well visualised throughout.
ii) limit the risk of carotid plaque rupture and subsequent stroke. -
The vagus nerve can be visualised within the carotid sheath. Local anaesthetic should be infiltrated around the carotid sheath, not within it.
-
DO NOT INJECT INTO THE CAROTID SHEATH.
-
The minimum volume of local anaesthetic needed for combined superficial cervical plexus and carotid blocks is 10 ml.
Other Resources
More information about carotid surgery can be found at the excellent free BJA article here
Text and images have been reproduced from the 2nd edition of the RA-UK Handbook, which can be purchased on Amazon, or is received on joining RA-UK. This excellent resource also contains practical descriptions of all of the advanced blocks referenced in the editorial.


 Introducing our brand new RAUK App. The free resource for all members to learn regional anaesthesia. Download the RAUK App on iOS or Android by clicking on the buttons..The App can be downloaded for free and non-members can view the Plan A content after registration. Members can unlock the full content by joining RA-UK where your RA-UK account will be linked.
Introducing our brand new RAUK App. The free resource for all members to learn regional anaesthesia. Download the RAUK App on iOS or Android by clicking on the buttons..The App can be downloaded for free and non-members can view the Plan A content after registration. Members can unlock the full content by joining RA-UK where your RA-UK account will be linked. 